Lower Extremity
Total Joints
What is total joint replacement?
An arthritic or damaged joint is removed and replaced with an artificial joint, called a prosthesis.
What is a joint?
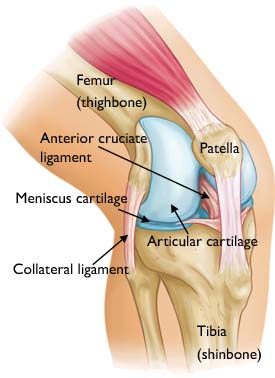
A joint is formed by the ends of two or more bones that are connected by thick tissues. For example, the knee joint is formed by the lower leg bone (tibia and fibula) and the thighbone (femur). The hip is a ball and socket joint, formed by the upper end of the femur (the ball), and a part of the pelvis, called the acetabulum (the socket).
The bone ends of a joint are covered with a smooth layer called cartilage. Normal cartilage allows nearly frictionless and pain-free movement. When the cartilage is damaged or diseased by arthritis, joints become stiff and painful. Every joint is enclosed by a fibrous tissue envelope or a capsule with a smooth tissue lining, called the synovium. The synovium produces fluid that reduces friction and wear in a joint.
Why is total joint replacement necessary?
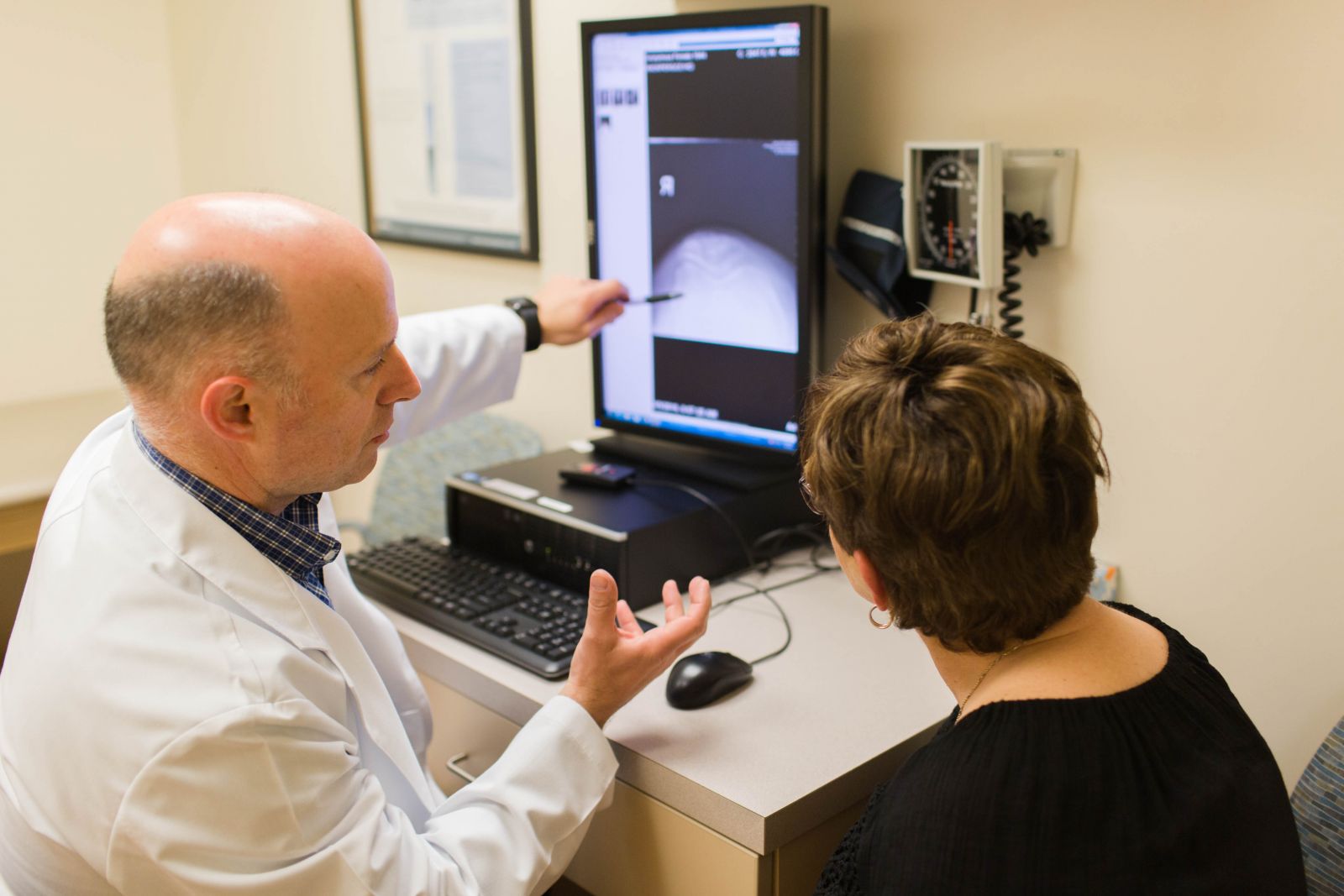
The goal is to relieve the pain in the joint caused by the damage done to the cartilage. The pain may be so severe, a person will avoid using the joint, weakening the muscles around the joint and making it even more difficult to move the joint. A physical examination, and possibly some laboratory tests and X-rays, will show the extent of damage to the joint. Total joint replacement will be considered if other treatment options will not relieve the pain and disability.
How is a total joint replacement performed?

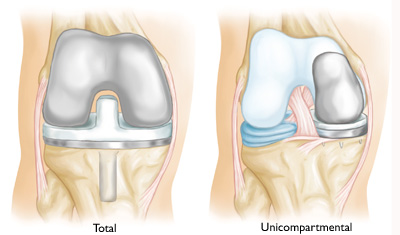
You will be given an anesthetic and the surgeon will replace the damaged parts of the joint. For example, in an arthritic knee the damaged ends of the bones and cartilage are replaced with metal and plastic surfaces that are shaped to restore knee movement and function.
In an arthritic hip, the damaged ball (the upper end of the femur) is replaced by a metal ball attached to a metal stem fitted into the femur and a plastic socket is implanted into the pelvis, replacing the damaged socket.
Although hip and knee replacements are the most common joint replaced, this surgery can be performed on other joints, including the ankle, foot, shoulder, elbow, and fingers.
The materials used in a total joint replacement are designed to enable the joint to move just like a normal joint.
The prosthesis is generally composed of two parts: a metal piece that fits closely into a matching sturdy plastic piece. Several metals are used, including stainless steel, alloys of cobalt and chrome, and titanium. The plastic material is durable and wear resistant (polyethylene). A plastic bone cement may be used to anchor the prosthesis into the bone.
Joint replacements also can be implanted without cement when the prosthesis and the bone are designed to fit and lock together directly.
What is the recovery process?
In general, your orthopaedic surgeon will encourage you to use your "new" joint shortly after your operation. After total hip or knee replacement, you will often stand and begin walking the day after surgery. Initially, you will walk with a walker, crutches, or a cane.
Most patients have some temporary pain in the replaced joint because the surrounding muscles are weak from inactivity and the tissues are healing. This will end in a few weeks or months.
Exercise is an important part of the recovery process. Your orthopaedic surgeon or the staff will discuss an exercise program for you after surgery. This varies for different joint replacements and for differing needs of each patient.
After your surgery, you may be permitted to play golf, walk, and dance. More strenuous sports, such as tennis or running, may be discouraged.
The motion of your joint will generally improve after surgery. The extent of improvement will depend on how stiff your joint was before the surgery.

What are the possible complications?
Tell your orthopaedic surgeon about any medical conditions that might affect the surgery. Joint replacement surgery is successful in more than 9 out of 10 people. When complications occur, most are successfully treatable.
Possible complications include the following.
Infection
Infection may occur in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home. It may even occur years later. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis.
Any infection in your body can spread to your joint replacement.
Blood Clots
Blood clots result from several factors, including your decreased mobility causing sluggish movement of the blood through your leg veins. Blood clots may be suspected if pain and swelling develop in your calf or thigh. If this occurs, your orthopaedic surgeon may consider tests to evaluate the veins of your leg. Several measures may be used to reduce the possibility of blood clots, including:
- Blood thinning medications (anticoagulants)
- Elastic stockings
- Exercises to increase blood flow in the leg muscles
- Plastic boots that inflate with air to compress the muscles in your legs
Despite the use of these preventive measures, blood clots may still occur. If you develop swelling, redness or pain in your leg following discharge from the hospital, you should contact your orthopaedic surgeon.
Loosening
Loosening of the prosthesis within the bone may occur after a total joint replacement. This may cause pain. If the loosening is significant, a revision of the joint replacement may be needed. New methods of fixing the prosthesis to bone should minimize this problem.
Dislocation
Occasionally, after total hip replacement the ball can be dislodged from the socket. In most cases, the hip can be relocated without surgery. A brace may be worn for a period of time if a dislocation occurs. Most commonly, dislocations are more frequent after complex revision surgery.
Wear
Some wear can be found in all joint replacements. Excessive wear may contribute to loosening and may require revision surgery.
Prosthetic Breakage
Breakage of the metal or plastic joint replacement is rare, but can occur. A revision surgery is necessary if this occurs.
Nerve Injury
Nerves in the vicinity of the total joint replacement may be damaged during the total replacement surgery, although this type of injury is infrequent. This is more likely to occur when the surgery involves correction of major joint deformity or lengthening of a shortened limb due to an arthritic deformity. Over time, these nerve injuries often improve and may completely recover.
How do you prepare for total joint replacement?
Before surgery, your orthopaedic surgeon will make some recommendations, such as suggesting that you:
- Donate some of your own blood so that, if needed, you may receive it during or after surgery
- Stop taking some drugs before surgery
- Begin exercises to speed your recovery after surgery
- Evaluate your need for discharge planning, home therapy and rehabilitation after surgery
Is total joint replacement permanent?
Most older persons can expect their total joint replacement to last a decade or more. It will give years of pain-free living that would not have been possible otherwise.
Younger joint replacement patients may need a second total joint replacement. Materials and surgical techniques are improving through the efforts of orthopaedic surgeons working with engineers and other scientists.
The future is bright for those who choose to have a total joint replacement to achieve an improved quality of life through greater independence and healthier pain-free activity.
Your orthopaedic surgeon is a medical doctor with extensive training in the diagnosis and nonsurgical and surgical treatment of the musculoskeletal system, including bones, joints, ligaments, tendons, muscles, and nerves.