Knee Degenerative Joint Disease
Degenerative joint disease of the knee is also known as osteoarthritis (OA). OA occurs when the cartilage that cushions your knee joint gradually deteriorates. Your odds of developing OA of the knee increase with advancing age, being overweight, having had previous injuries to the joint, and having a genetic predisposition to the development of OA. Osteoarthritis is a degenerative disease that worsens over time. Symptoms can include joint pain, stiffness, or a sense of grinding in the joint.
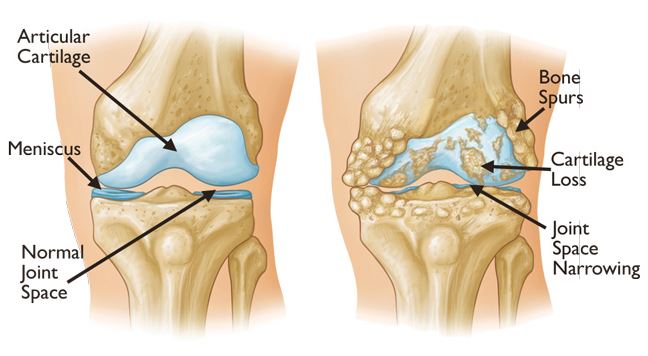
Osteoarthritis is diagnosed by physical evaluation and x-rays. An MRI is not commonly required for this diagnosis. There are things you can do to slow the progression of joint deterioration including staying active and maintaining a healthy weight. Other conservative measures include use of viscosupplementation injections which may use steroid medication to decrease inflammation and relieve pain or may use hyaluronic acid to provide joint lubrication. These lubricating injections include Synvisc, Euflexxa, and Zilretta, to name a few. The doctor may also recommend use of a non-steroidal anti-inflammatory medication. A physical therapist can provide pain-relieving treatments such as ultrasound or electrical stimulation and will teach you exercises to stretch tight muscles, improve joint stiffness, and strengthen the muscles that support the knee.
Once the osteoarthritis progresses to the point that conservative treatments no longer provide relief of symptoms, surgical intervention may be an option. In joint replacement surgery, the surgeon will remove the damaged joint surfaces and replace them with plastic and metal parts. This type of surgery typically requires an overnight hospital stay. If you are diabetic, it is important to maintain healthy sugar levels after surgery to decrease likelihood of developing adhesive capsulitis (frozen knee). Smoking also increases your risk of developing this issue. Adhesive capsulitis sometimes requires an arthroscopic surgery to release scar tissue that is keeping the knee from bending and straightening properly.
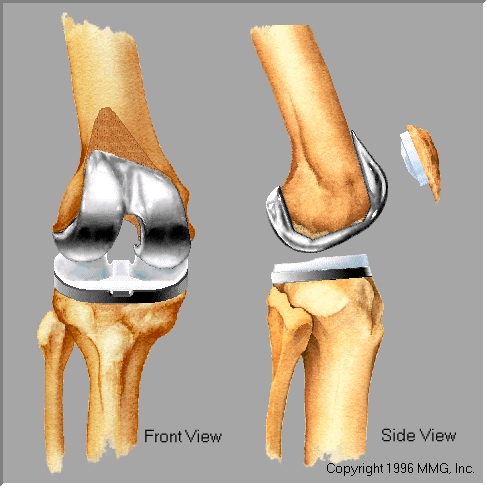
Rehab following knee replacement is extremely important for regaining full range of motion at the knee and to help you achieve good mobility. If you rest and try to avoid pain in the days and weeks after surgery, you will likely end up with a very stiff knee and have difficulty performing mobility tasks such as stair climbing and getting out of a chair. In the first days after surgery, it will be painful to move the knee. If you push through the pain to perform your range of motion and stretching exercises, these exercises will actually provide relief of pain and of stiffness with activity. In addition, the doctor may order a continuous passive motion (CPM) machine that will be used for a total of 6 hours per day in 2 hour increments. This machine will passively bend and straighten your knee.
The most common complaint after knee replacement is that the new knee gets very stiff after a period of rest. The best way to limit this stiffness is to keep the knee moving and stay active during the day. If you are homebound, physical therapy services can be provided in your home. If not, you can be treated on an outpatient basis. People who are compliant with their exercise program and with use of the CPM machine are typically discharged from physical therapy within 4-8 weeks of surgery.
Total Joint Replacement FAQ
Will I Stay in the Hospital After Surgery?
You can plan on at least 1 night in the hospital after surgery. Sometimes patients need to stay 2-3 nights. Some patients choose to go to a skilled care facility, or a swing bed facility. Most go home upon discharge. You will need to have a responsible adult at your home for the first week or so.
Insurance has specific requirements patients must meet in order to be accepted into a skilled care facility,inpatient rehab, or swing bed facility. Please be aware that Medicare may not cover a skilled nursing facility stay following elective surgery. Coverage typically depends on meeting specific medical criteria, including a qualifying inpatient hospital stay and a demonstrated need for skilled care.
Once home, we will order Home Health Services. If approved through your insurance, a Nurse and Physical Therapist will visit you a few times a week once you arrive home. They may request further services, like Occupational Therapy.
Outpatient Physical Therapy will be ordered for you to attend at a facility of your choice after you are released from Home Health, or if Home Health is not approved through your insurance. You will have outpatient physical therapy for about 6 weeks after surgery. Physical therapy is VERY important to your healing process.
Will I Need Equipment at Home? What About Medication?
Yes. You will need a walker, and perhaps other equipment, like a bedside commode or toilet riser. Total Knee arthroplasties are ordered a continuous range of motion device (CPM) or ROMTECH device. The equipment will be ordered for you by the Social Worker at the hospital prior to your discharge based on your type of surgery. They can be picked up at a local equipment store.
When you leave the hospital, you will be ordered pain medication and a blood thinner. These will be sent to the pharmacy of your choice. The Blood thinner is a very important medication for you to take. It will help prevent blood clots, otherwise known as deep vein thrombus (DVT), which is a potential complication after a total joint surgery. Sometimes the blood thinner can be expensive at the pharmacy. If this happens, we have access to coupons or samples.
When Will I Need to Follow Up in Your Office After Surgery?
You will see a provider 2 weeks after surgery. Then you will be seen at 6 weeks, 12 weeks and 1 year after surgery. We will obtain Xrays and evaluate your healing, progress and address any concerns you may have. If you have a total hip arthroplasty, you will not have any sutures or staples to be removed. If you have a total knee arthroplasty, the clinic staff will remove your staples at your first post operative appointment.
When Can I Drive After Surgery?
As long as you drove prior to surgery, you can expect to be able to drive after surgery at about 4-6 weeks post op. This will depend on if you had the right or left leg operated on, if you drive an automatic or manual vehicle. You will not be released to drive if you are still taking narcotics.
What Do I Ned to do to Prepare for Surgery?
You will need pre operative clearance from your medical provider. If you see a cardiologist, we will need clearance from them as well. Our surgical scheduler will send your family physician/cardiologist the clearance form to be completed, but you will need to schedule an appointment with your family physician to get it completed.
You will be required to attend a Total Joint class at Good Samaritan Hospital . The class is led by one of the nurses at the hospital. She will give you information on the surgical process and can answer a lot of questions you may have regarding your hospital stay. At this class, you will meet with the hospital case manager supervisor/social worker, home health nurse to learn about postoperatiave therapies and services.
Is There Anything I Need to Know After My Surgery?
Yes! After surgery, we would like you to postpone any non urgent dental appointments for 3 months. Of course, if you have something urgent that needs taken care of, please do so. After the initial 3 months, if you do have a dental appointment, we require you to take pre-dental antibiotics. This is to help prevent any infection. We also will order you pre-procedure antibiotics if you need to have any gastrointestinal procedures, like a colonoscopy. Just call our office and let us know before your appointment and our nurses will send the antibiotics in to your pharmacy.
What Things Are Normal After Surgery?
You may hear a click when you walk. This is normal. You may notice the operative leg is more swollen or warm to touch than the other leg. Swelling and warmth can be normal for a period of time after surgery. You had a big surgery! However, if you ever have concerns about ANYTHING in your post operative period, we are available to talk to you.
Are There Any Things to Look For After Surgery?
Calf pain, calf swelling, calf redness, feeling like you have a Charlie horse- these can be signs of a blood clot. Doing range of motion,walking, taking the blood thinner, and wearing the TED hose can help prevent this risk. Constipation can occur after surgeries, especially if you are taking a narcotic. An over the counter stool softner such as Colace, Ducolox or Miralax can help, as will staying hydrated and eating fiber rich foods. Not having a bowel movement can be very uncomfortable, but also can become a big issue if not resolved.
If you were to experience any of these complications, we would ask you to call our office at 618-242-3778. If after hours or the weekend call the hospital at 618-242-4600 to have the hospital page our on call surgeon, or go to the Emergency Room for treatment.
Infection, Blood clots and constipation are 3 things we would like you to keep your eye out for after surgery.
We will ask you to monitor yourself for signs and symptoms of infection, things like fever, chills, foul odor, drainage.