Trigger Finger Vs. Dupuytren's Contracture
Trigger finger and Dupuytren's contracture are both problems that affect the fingers and so one issue is often confused for the other.
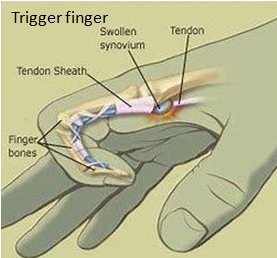
On the palmar side of each finger, there is a tendon that helps each finger bend toward the palm. Each of these tendons is surrounded by a sheath which is lined with synovium. Synovium produces a fluid that allows the tendon to glide easily as you bend and straighten your finger.
In the case of trigger finger, one of these tendons becomes inflamed and the tendon or the sheath surrounding it can swell and thicken to the point that the tendon can no longer glide smoothly. Because of this, when you try to straighten the finger, the tendon catches and can "trigger" into a bent position as it tries to squeeze back through the sheath. Diagnosis is typically made by physical examination by the physician. You may be asked to make a fist and then straighten your fingers. In the case of trigger finger, the affected finger may stay curled or may suddenly pop out straight. You may have to straighten the bent finger with your other hand. The palm of the hand contains a fibrous layer of tissue called the palmar fascia. The palmar fascia acts as a protective barrier between the skin and the tendons that help to bend the fingers toward the palm.
In the case of Dupuytren's contracture, the palmar fascia thickens and draws in which causes the affected finger to bend toward the palm. Small hard knots can form just under the skin at the base of the finger. The ring and little fingers are most commonly affected. Diagnosis of Dupuytren's contracture is made by physical examination by the physician. Knots at the base of the affected fingers and scarlike bands across the palm are obvious signs, as is the inability to lay the hand down flat on a surface. Unlike a finger which is bent due to trigger finger, a finger bent by Dupuytren's contracture is unable to straighten, even with help from the other hand.
Trigger finger can be treated conservatively in mild cases, with treatment options including use of an oral anti-inflammatory medication or injection of cortisone. Injection can be used up to 3 times for treatment of a trigger finger, but the issue is resolved after the first injection in 80% of cases. If conservative measures fail to improve symptoms, surgery may be recommended. Surgery for trigger finger involves opening the tendon sheath to enlarge the space and release the swollen tendon. This allows the finger to bend and straighten again. Surgery is often done using local anesthesia on an outpatient basis. Sutures are removed 2 weeks after surgery. Light activity is allowed after 1-2 weeks while heavy manual labor is allowed after 4-6 weeks.
Dupuytren's contracture cannot be treated with conservative measures so surgery is often recommended. Dr. Ahn typically recommends surgery for Dupuytren's contracture once it adversely affects use of the hand. When the case is severe enough for surgery, patients often report being unable to get the hand in a pocket and/or having the affected finger poke the eye while trying to wash the face. This surgery is performed under general anesthesia on an outpatient basis. During surgery, the section of the palmar fascia containing the nodules is removed. This allows you to regain better finger motion. After surgery, a splint is worn for the first week. Sutures are removed after 3 weeks. In some cases, occupational therapy may be recommended for finger range of motion and scar massage. Patients undergoing this surgery are allowed to return to regular activity after 6 weeks.